As the founder of LEAD Ministries and an advocate for child rights, I feel compelled to raise urgent alarm about a disturbing global trend: the for
Study proves strong impact of taking molecular TB diagnostics closer to the people. By SHOBHA SHUKLA, BOBBY RAMAKANT

Study proves strong impact of taking molecular TB diagnostics closer to the people. Urgent call to replace sputum microscopy completely with true point-of-care molecular tests to #FindAllTB
An important scientific study published in The Lancet shows the strong public health impact of deploying molecular diagnostics closer to the people.
This multi-country randomised controlled study shows that if we deploy battery-operated, laboratory independent and true point-of-care molecular test Truenat at the primary healthcare level, then same day test and treat can become a reality. Diagnosing TB early and accurately is a critical pathway towards right treatment as well as stopping the spread of infection.
The study enrolled around 4000 participants in 29 primary healthcare clinics of Tanzania and Mozambique during August 2022 and June 2023. In one study-arm, 2007 participants were accessing primary healthcare clinics equipped with point-of-care molecular test Truenat. In the second study-arm, 1980 people were served by primary healthcare clinics with no molecular test, but their samples were collected and sent to a laboratory with molecular test Gene Xpert (11-16 km away) and their test reports transported back. Both these molecular tests are WHO recommended ones.
Same day test and treat becomes a reality for 4-in-5 TB patients when POC tests deployed
The study found that 97% of TB patients could begin treatment within 7 days when point-of-care Truenat was deployed at the primary care level. But only 63% could do so when samples were sent to a remote lab where Gene Xpert was deployed.
More importantly, 82.2% of the TB patients who were diagnosed with Truenat at the primary care level, could be initiated on right TB treatment on the same day – so, same day test and treat could become a reality in remote peripheral settings. But only 3% could get same day treatment initiation if tested by Gene Xpert deployed in a remote lab.
Study authors categorically state that “this study provides strong evidence supporting the placement of low complexity molecular TB diagnostics at primary care level, to enable same-day diagnosis and treatment initiation.”
TB deaths were 3-fold among those who were in the study-arm where samples were to be sent to a remote lab equipped with Xpert (2.1%) compared to those who were in the study-arm with Truenat deployed at the primary care level (0.7%). Eliminating diagnostic delays and delays between diagnosis and treatment can save lives.
By not deploying point-of-care molecular TB tests we are programming to fail on "same day test and treat" too – and thereby failing to reduce unnecessary human suffering and risk of untimely death due to TB. Also, we cannot break the chain of infection transmission unless we diagnose TB early and accurately and initiate right treatment without any delay.
1.5 times more people began treatment within 7 days when POC molecular test deployed at primary care level
Study authors observed that “we found that the placement of the Truenat platform with MTB Plus and MTB-RIF Dx assays at clinics combined with rapid communication of results and same-day TB treatment initiation led to a 1.5 times higher proportion of people starting treatment for microbiologically confirmed TB within 7 days.”
It is also important to note that study researchers had found major problems with sputum transport systems which negatively impacted the TB programme. Study authors noted that “study site assessments revealed operational issues [with Gene Xpert] (for example, sputum container stockouts and delays in sample transport) leading to occasional referral of patients instead of samples. To address this issue, sputum containers were stocked throughout, and samples were collected at least twice weekly. Off-site laboratories received Xpert MTB/RIF Ultra cartridges for sample testing.”
So, even if so-called hub-and-spoke model or sputum referral system works 'perfectly' (like in this study) then too TB programme outcomes are majorly compromised. One can imagine when real life problems mar this hub-and-spoke model then TB programme outcomes would be getting even more compromised.
In the study-arm where Truenat was deployed at the primary care level, it took an hour to find if a person has active TB disease (and if so, then whether the TB bacteria is resistant to one of the two most effective anti-TB medicines, rifampicin). The person was asked to wait for one hour and if found positive for TB, then treatment could be initiated on the same day for over 82% patients.
This Lancet publication co-authored by Dr Celso Khosa of Instituto Nacional de Saúde in Mozambique, Dr Adam Penn-Nicholson of FIND in Geneva, and other researchers from several medical and scientific institutions, is among the very few studies that have compared the difference it makes by deploying molecular diagnostics at primary care level with off-site remote laboratory with centralised or semi-centralised molecular testing (and samples sent to the lab and reports back to the peripheral clinic). Most other studies have compared the difference between a bad TB upfront test (sputum microscopy, which badly underperforms in diagnosing TB) at primary care level with off-site molecular testing.
Truenat molecular test is also the largest used molecular test deployed in India - a nation home to world's largest number of people with TB. It is deployed in over 90 countries now. For example, the largest rollout of Truenat in Africa took place last year in Nigeria with AI-enabled handheld X-Rays and solar-power charging capabilities in remote peripheral areas.
Replace microscopy with 100% upfront POC molecular TB test
Ahead of the world’s biggest TB and lung disease conference (Union World Conference on Lung Health) that will be held next month, this study published in the Lancet provides potentially groundbreaking scientific evidence for high TB burden countries on the major difference it makes by deployment of WHO recommended point-of-care molecular test Truenat at the primary care level.
If we are to serve the underserved, take best of healthcare and social support services with equity, rights and human dignity.
If we are to end TB we cannot afford any delays - be they diagnostic delays or delays spanning many days between diagnosis and initiation of treatment. Moreover, deploying point-of-care health technologies at the point-of-need helps break the barriers people face in accessing centralised healthcare services.
All world leaders at the United Nations General Assembly High Level Meeting on TB in 2023 had committed to completely replace microscopy with upfront molecular TB tests by 2027. With the light this study shines on bringing molecular tests to the primary care level, all efforts must be full throttle to replace microscopy with point-of-care molecular tests that are deployable in high-burden settings.
Do away with hub-and-spoke model when every spoke can be a hub
Study authors stated: “Although Xpert MTB/RIF, endorsed by WHO in 2011, revolutionised TB and rifampicin resistance detection, its impact has been limited. High costs and operational requirements (eg, stable electricity, temperature control, and dust-free environments) have confined its use to centralised laboratories in hub-and-spoke models. New molecular and point-of-care diagnostics are emerging that might be deployed in primary care clinics or even in communities. Portable battery-operated molecular testing platforms, such as the Molbio Truenat platform (endorsed by WHO in 2020), offer the potential to further decentralise molecular testing.”
This randomized control study provides pathbreaking science to call for transforming every 'spoke' into a hub by deploying WHO recommended point-of-care molecular tests like Truenat which are battery-operated (with solar power recharging capabilities), laboratory independent, and decentralised. More importantly, it is a multi-disease molecular testing platform for over 40 diseases, such as TB, HIV (including viral load, testing) hepatitis B and C virus, human papilloma virus (HPV - which causes a lot of cervical cancers), several sexually transmitted infections, leprosy, vector-borne diseases like malaria, among others.
Earlier this week while launching an important WHO report on antimicrobial resistance, WHO Director General Dr Tedros Adhanom Ghebreyesus too had underpinned the importance of "rapid and point-of-care molecular testing" for preventing AMR - because correct and timely diagnosis for multiple diseases must be made accessible to all equitably - especially those who are underserved. Linkage to standard treatment, care and support also should be made accessible to all if we are to prevent AMR, along with optimal infection prevention and control, vaccination, water, sanitation and hygiene, and other health and social support.
(Shobha Shukla is the founding Managing Editor of CNS (Citizen News Service) and Bobby Ramakant works as CNS Health Editor. Both are on the boards of Global Antimicrobial Resistance Media Alliance (GAMA) and Asia Pacific Media Alliance for Health, Gender and Development Justice (APCAT Media). Follow them on Twitter/X: @Shobha1Shukla, @BobbyRamakant, @CNS_Health)
You May Also Like
Even before 2026 began, we were never on track to deliver on gender equality and human right to health and broader development justice. For e
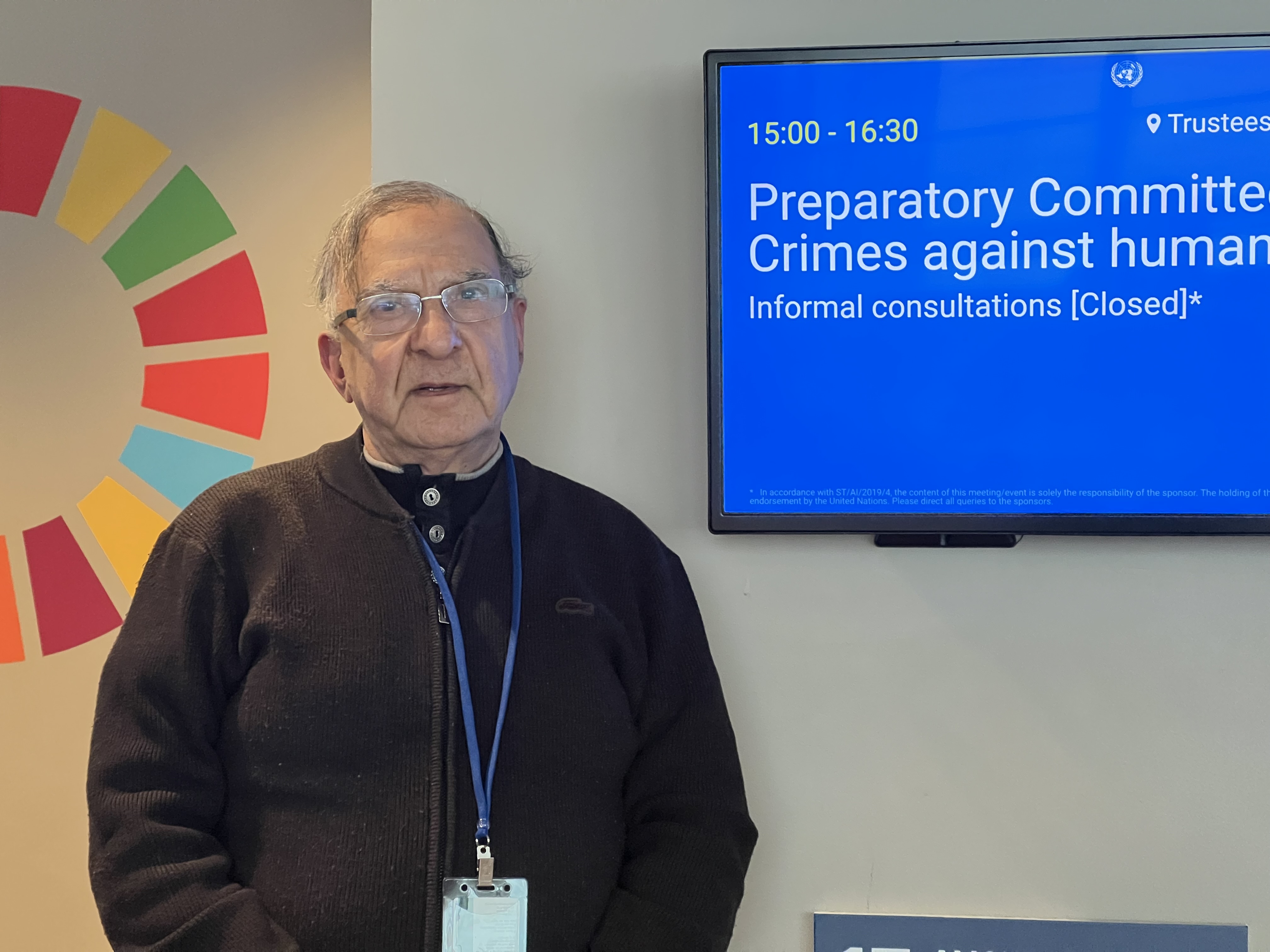
New York: Crimes against humanity represent one of the most serious affronts to human dignity and collective conscience. They embody patterns of wi

"Trial of Pakistani Christian Nation" By Nazir S Bhatti
On demand of our readers, I have decided to release E-Book version of "Trial of Pakistani Christian Nation" on website of PCP which can also be viewed on website of Pakistan Christian Congress www.pakistanchristiancongress.org . You can read chapter wise by clicking tab on left handside of PDF format of E-Book.