As the founder of LEAD Ministries and an advocate for child rights, I feel compelled to raise urgent alarm about a disturbing global trend: the for
New Scientific Strategy In The Quest For An HIV Cure. By Shobha Shukla

A Global Scientific Strategy Towards an HIV Cure, developed by a group of 34 leading HIV scientists and clinicians on behalf of the International AIDS Society (IAS), was launched in Washington DC on 19th July, 2012, ahead of the XIX International AIDS Conference amid renewed optimism that prospects for finding an HIV cure are increasing. The vision for the IAS strategy is that a safe, affordable and scalable cure for HIV will improve the health and quality-of-life for those with living with the infection, and reduce the risk of transmission of virus to those not infected. The strategy identifies seven important priority areas for basic, translational and clinical research and maps out a path for future research, collaboration and funding opportunities.
According to Dr Françoise Barré-Sinoussi, the co-discoverer of HIV, Director of the Regulation of Retroviral Infections Unit at the Institut Pasteur in Paris and the IAS President-Elect, “The strategy is the result of a collaborative effort which has produced a roadmap that will constructively move HIV Cure research forward.”
“What we haven’t had until very recently is clear insights into why HIV persists during therapy,” said Professor Steven Deeks, Professor of Medicine at the University of California, San Francisco, at the launch in Washington, D.C. “Our basic understanding of the mechanisms of HIV persistence in latent reservoirs is far superior than it was a decade ago. We are entering a stage in the epidemic in which we can seriously begin testing drugs that either prevent latency or which force the virus out of its hiding place, make it susceptible to our current drugs.”
Major investments in science have resulted in the worldwide availability of over 20 anti-HIV drugs which can restore health, prolong life and reduce transmission of the virus. HIV-infected individuals who have access to antiretroviral drugs, and who are able to adhere to therapy can maintain control of HIV infection indefinitely. Despite these successes, these therapies cannot eradicate HIV, requiring people to remain on expensive and potentially toxic drugs for life and also remain prone to co-morbidities. Although the cost of delivering antiretroviral drugs to the more than 34 million people now living with HIV has decreased substantially, it is still overwhelmingly high. Estimates put the cost of the funding response to the HIV/AIDS epidemic by 2015 between US$22-24 billion per year and between US$19-35 billion per year by 2031, with antiretroviral treatment accounting for up to 70 per cent of the total cost of care in the most affected countries.
Thus the search for an HIV Cure is an imperative in terms of the individual and public health benefits and an opportunity to potentially avoid the long-term cumulative costs of ART. An effective and scalable HIV cure is likely to stop transmission of HIV to those who are uninfected and restore the immunological function and normal health to those who are infected.
Many scientific advances are helping to shed light on why it is that HIV remains persistent.
Scientists have known for some time now that latent HIV reservoirs, where HIV hides and persists, are one of the main barriers to finding a cure. This is precisely why treatment does not eradicate HIV and when treatment is stopped, the virus rebounds.
For the first time now there is a “proof of concept,” for an effective cure. The case of Timothy Brown, the so-called “Berlin Patient”, who received a stem-cell bone-marrow transplant in 2007 and as he lacked CCR5, (the doorway through which HIV enters cells), is now considered to be cured of HIV and has got scientists thinking about the use of gene therapy to modify a patient’s own immune cells to make them resistant to HIV infection. The molecular biology regarding how HIV DNA becomes integrated in the chromosomes of infected people is the focus of intense research leading to a number of possible interventions, some of which are being tested in the clinic. Recently, in a test in HIV+ patients, scientists have shown that a dose of a drug, that inhibits an enzyme involved in HIV silencing, leads to rapid production of HIV RNA in the patient’s latently infected cells. This could make such previously unreachable viral reservoirs susceptible to curative strategies. Scientists are also gaining a better understanding of a rare group of HIV infected people who appear to have naturally “cured” their own infection. These “elite controllers” are HIV positive but have no readily apparent virus in the blood. Scientists are.
There exists a unique cohort of patients in France who became HIV infected, started therapy early, and were able to successfully stop therapy without viral rebound (the “Visconti Cohort”). The study confirms the benefits of treating HIV at the very early stages of infection. Understanding this group of people, who efficiently control the virus replication and reservoirs, might lead to novel therapeutic interventions.
Currently, the following strategies are being investigated and it is expected that all of these strategies will be more efficient in combination with each other, alongside the use of antiretroviral therapy to at least protect the immune system of patients to prepare them for a cure:
(i)Gene therapy; (ii)Treatment Optimization and Intensification (iii)Reversal of HIV; (iv) Immune-based Therapies and (v)Therapeutic Vaccination
Strong community support is needed to advocate against complacency and to ensure that patients and their communities are fully engaged and informed about the risks and benefits of curative studies. “Under no circumstances should the inclusion of “cure” in the global response direct funding away from treatment, prevention and care programmes, or from biomedical research on HIV and its consequences, including vaccine and other prevention research,” said Barré-Sinoussi. “However, it is imperative that donors, governments and the AIDS community make viable economic investment in HIV cure research, and right now.”
(The author is the Managing Editor of Citizen News Service (CNS). She is a J2J Fellow of National Press Foundation (NPF) USA. She has worked earlier with State Planning Institute, UP and taught physics at India's prestigious Loreto Convent. She also authored a book on childhood TB (2012), co-authored a book (translated in three languages) "Voices from the field on childhood pneumonia" and a report on Hepatitis C and HIV treatment access issues in 2011. Email: shobha@citizen-news.org, website: http://www.citizen-news.org)
According to Dr Françoise Barré-Sinoussi, the co-discoverer of HIV, Director of the Regulation of Retroviral Infections Unit at the Institut Pasteur in Paris and the IAS President-Elect, “The strategy is the result of a collaborative effort which has produced a roadmap that will constructively move HIV Cure research forward.”
“What we haven’t had until very recently is clear insights into why HIV persists during therapy,” said Professor Steven Deeks, Professor of Medicine at the University of California, San Francisco, at the launch in Washington, D.C. “Our basic understanding of the mechanisms of HIV persistence in latent reservoirs is far superior than it was a decade ago. We are entering a stage in the epidemic in which we can seriously begin testing drugs that either prevent latency or which force the virus out of its hiding place, make it susceptible to our current drugs.”
Major investments in science have resulted in the worldwide availability of over 20 anti-HIV drugs which can restore health, prolong life and reduce transmission of the virus. HIV-infected individuals who have access to antiretroviral drugs, and who are able to adhere to therapy can maintain control of HIV infection indefinitely. Despite these successes, these therapies cannot eradicate HIV, requiring people to remain on expensive and potentially toxic drugs for life and also remain prone to co-morbidities. Although the cost of delivering antiretroviral drugs to the more than 34 million people now living with HIV has decreased substantially, it is still overwhelmingly high. Estimates put the cost of the funding response to the HIV/AIDS epidemic by 2015 between US$22-24 billion per year and between US$19-35 billion per year by 2031, with antiretroviral treatment accounting for up to 70 per cent of the total cost of care in the most affected countries.
Thus the search for an HIV Cure is an imperative in terms of the individual and public health benefits and an opportunity to potentially avoid the long-term cumulative costs of ART. An effective and scalable HIV cure is likely to stop transmission of HIV to those who are uninfected and restore the immunological function and normal health to those who are infected.
Many scientific advances are helping to shed light on why it is that HIV remains persistent.
Scientists have known for some time now that latent HIV reservoirs, where HIV hides and persists, are one of the main barriers to finding a cure. This is precisely why treatment does not eradicate HIV and when treatment is stopped, the virus rebounds.
For the first time now there is a “proof of concept,” for an effective cure. The case of Timothy Brown, the so-called “Berlin Patient”, who received a stem-cell bone-marrow transplant in 2007 and as he lacked CCR5, (the doorway through which HIV enters cells), is now considered to be cured of HIV and has got scientists thinking about the use of gene therapy to modify a patient’s own immune cells to make them resistant to HIV infection. The molecular biology regarding how HIV DNA becomes integrated in the chromosomes of infected people is the focus of intense research leading to a number of possible interventions, some of which are being tested in the clinic. Recently, in a test in HIV+ patients, scientists have shown that a dose of a drug, that inhibits an enzyme involved in HIV silencing, leads to rapid production of HIV RNA in the patient’s latently infected cells. This could make such previously unreachable viral reservoirs susceptible to curative strategies. Scientists are also gaining a better understanding of a rare group of HIV infected people who appear to have naturally “cured” their own infection. These “elite controllers” are HIV positive but have no readily apparent virus in the blood. Scientists are.
There exists a unique cohort of patients in France who became HIV infected, started therapy early, and were able to successfully stop therapy without viral rebound (the “Visconti Cohort”). The study confirms the benefits of treating HIV at the very early stages of infection. Understanding this group of people, who efficiently control the virus replication and reservoirs, might lead to novel therapeutic interventions.
Currently, the following strategies are being investigated and it is expected that all of these strategies will be more efficient in combination with each other, alongside the use of antiretroviral therapy to at least protect the immune system of patients to prepare them for a cure:
(i)Gene therapy; (ii)Treatment Optimization and Intensification (iii)Reversal of HIV; (iv) Immune-based Therapies and (v)Therapeutic Vaccination
Strong community support is needed to advocate against complacency and to ensure that patients and their communities are fully engaged and informed about the risks and benefits of curative studies. “Under no circumstances should the inclusion of “cure” in the global response direct funding away from treatment, prevention and care programmes, or from biomedical research on HIV and its consequences, including vaccine and other prevention research,” said Barré-Sinoussi. “However, it is imperative that donors, governments and the AIDS community make viable economic investment in HIV cure research, and right now.”
(The author is the Managing Editor of Citizen News Service (CNS). She is a J2J Fellow of National Press Foundation (NPF) USA. She has worked earlier with State Planning Institute, UP and taught physics at India's prestigious Loreto Convent. She also authored a book on childhood TB (2012), co-authored a book (translated in three languages) "Voices from the field on childhood pneumonia" and a report on Hepatitis C and HIV treatment access issues in 2011. Email: shobha@citizen-news.org, website: http://www.citizen-news.org)
You May Also Like
Even before 2026 began, we were never on track to deliver on gender equality and human right to health and broader development justice. For e
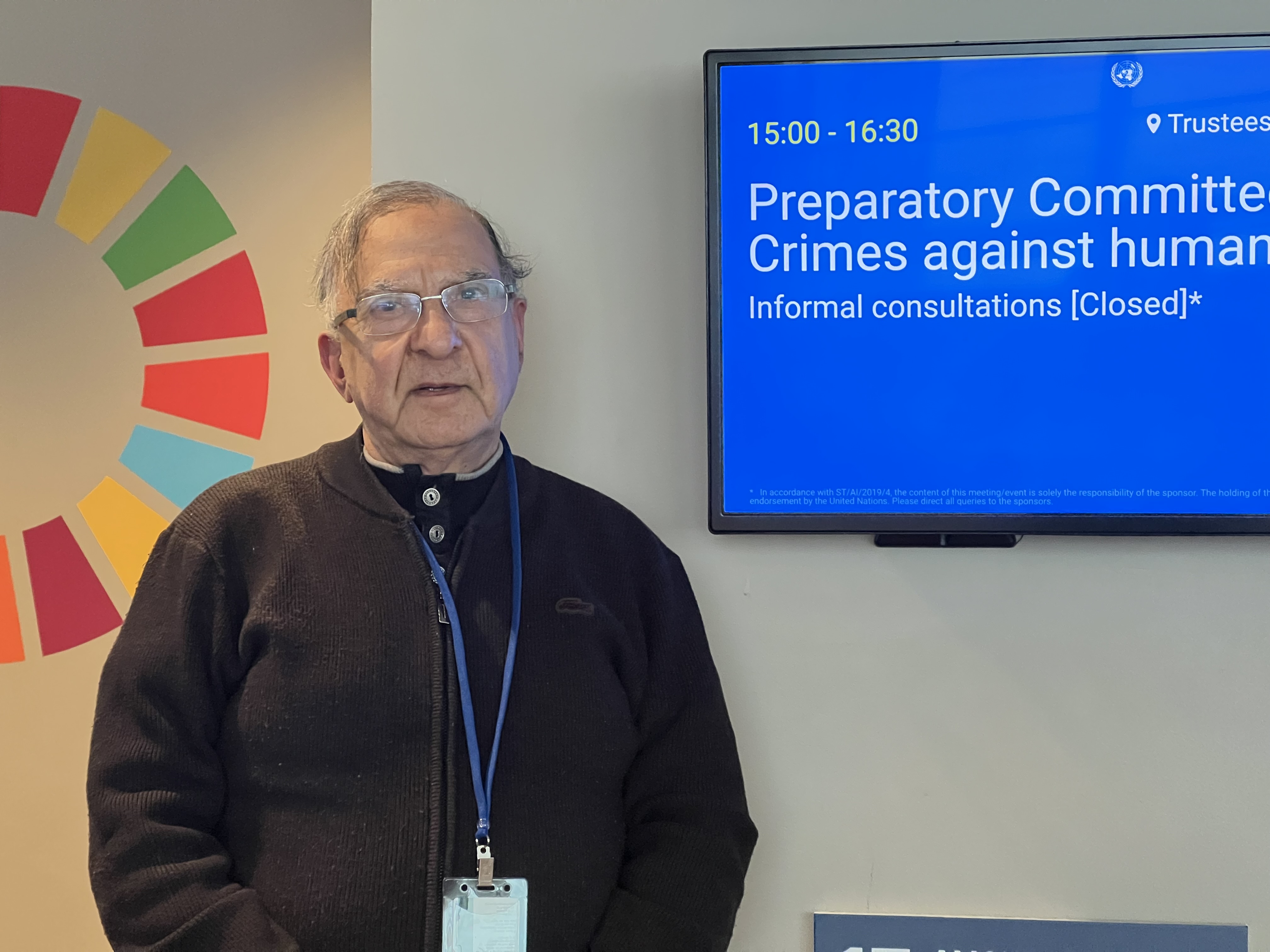
New York: Crimes against humanity represent one of the most serious affronts to human dignity and collective conscience. They embody patterns of wi

"Trial of Pakistani Christian Nation" By Nazir S Bhatti
On demand of our readers, I have decided to release E-Book version of "Trial of Pakistani Christian Nation" on website of PCP which can also be viewed on website of Pakistan Christian Congress www.pakistanchristiancongress.org . You can read chapter wise by clicking tab on left handside of PDF format of E-Book.